Abstract
Introduction
Diffuse large B cell lymphoma (DLBCL) is the most common type of non-Hodgkins lymphoma (NHL), constituting 25% of NHL cases. (CA Cancer J Clin PMID: 27618563) Patients with aggressive hematological malignancies (HM) including lymphomas and leukemias have substantial palliative care needs that entail symptoms management and Hospice as an essential component of end of life (EoL) care. Despite significant improvement in treatment options, patients with relapsed refractory (RR) HM have suboptimal EoL care, (Blood PMID: 28774879 and Hematology Am Soc Hematol Educ Program PMID: 33275720) compared to patients with solid malignancies. (J Clin Oncol PMID: 25154824) The purpose of this study was to assess for Hospice enrollment in patients with DLBCL within the Veterans Health Administration (VHA).
Methods
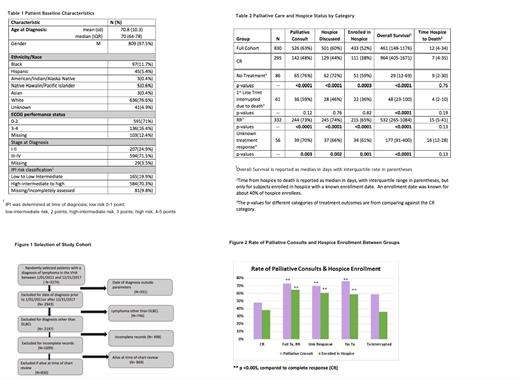
Trained abstractors performed a retrospective chart review of 3274 randomly selected patients with an ICD code for lymphoma treated within the VHA between 01/01/2011 and 12/31/2017. During the study period, 1699 veterans were confirmed to have a diagnosis of DLBCL, out of which 830 deceased patients were analyzed for this study. (Figure 1) Rates of palliative care consults, Hospice discussions, and Hospice enrollment were compared by age, race and outcomes of first line treatments using the Chi-Squared test of independence. Overall survival (OS) and time from Hospice to death were compared for the same variables with the Wilcoxon-Mann-Whitney test. A significance level of 0.05 was used for this study and all tests were two-tailed.
Results
The median age at diagnosis was 70 years. The predominant population was white males. At the time of diagnosis, approximately three fourths had an ECOG performance status of 0 to 2. Over 50% were diagnosed at stage III-IV and had an IPI score of 4 or 5. (Table 1) Within the study, 63%, 60% and 52% of patients were introduced to palliative care, had Hospice discussions, and enrolled in Hospice respectively. The median OS from date of diagnosis to death was 461 days, and the median time from Hospice enrollment to death for those with a known Hospice enrollment date was 12 days. (Table 2) There was no statistically significant difference in palliative care or Hospice usage, median OS or median time in Hospice to death, by age or race. Patients with complete response (CR) to first line treatment had longer median OS in comparison to the four other groups: patients who received no first line treatments, who began a first line treatment which was interrupted by death, who were RR after first line treatment and those with an unknown treatment response. Patients who did not receive any first line treatments, RR patients or those with an unknown treatment response were more likely to have a palliative care consult, discuss Hospice with a provider and enroll in Hospice (p-value <0.005). There were no statistically significant differences in median time within Hospice between the successful treatment group and any of the other four groups.
Conclusion
In this retrospective study, more than half of deceased patients with DLBCL within the VHA utilized Hospice services. There was no difference in Hospice use based on age or race, indicating equal access to care. Limitations of this study include a predominant male population and equal health care access that may limit generalizability of our finding to the non-Veterans population. Early recognition of high-risk patients may correlate with earlier enrollment to Hospice and increased lengths of stay in Hospice for patients with aggressive HM. Future educational interventions are needed to improve Hospice utilization for EoL care in patients with HM.
Nooruddin: AstraZeneca: Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal